AI and Clinical Coaching support patients improve self-management of long-term conditions
Written by: Ellen Barnes - 9th July 2021
 In this blog, our Programme Manager Ellen Barnes talks about how HN has developed an innovative programme to support individuals most at risk of becoming acutely unwell.
In this blog, our Programme Manager Ellen Barnes talks about how HN has developed an innovative programme to support individuals most at risk of becoming acutely unwell.
Another project within the NHSX Joined Up Care Programme is the Complex Needs Virtual Ward project, which aims to reduce the volume of A&E attendances across multiple morbidities (patients living with two or more chronic illnesses). HN aims to reduce this by identifying high risk patients and giving them specific health coaching support before they become high users of unplanned/emergency care.
I mentioned in my previous blog –‘Protecting the vulnerable with digital innovation’– that prevention is better than cure, but what happens when it’s not necessarily a cure and more about living with and managing long-term conditions? There can be an overwhelming amount of information and support a patient needs before being comfortable managing their condition or multiple conditions and their needs will change over time. We can all appreciate that no two individuals are the same or have the same needs. So how can digital innovation help here?
Well, HN (previously Health Navigator) has developed a combined solution for patients with complex multiple needs, utilising best of both: artificial intelligence (AI) and personalised care. HN has developed an AI algorithm which looks at patient data and identifies those patients at risk of becoming increased users of clinical services (predictive analytics).
Process flow for AI-guided Clinical Coaching:
EPRs – Electronic Patient Records PROMs – Patient Reported Outcome Measures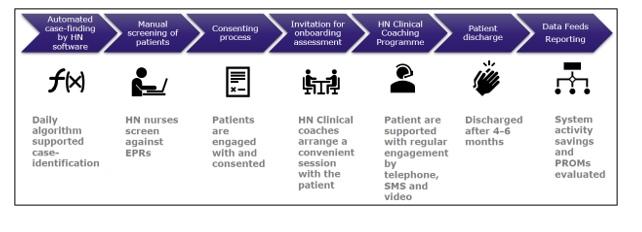
Patients who are invited to take part in the service are then screened and have access to a clinical coach. Clinical Coaching is a telephone-based nurse-led service, providing sessions to empower the patient and improve care coordination with other services.
Initially, contact can be many times per week, then tailored to patients’ needs. The support is offered over a two-year period, but patients would usually only remain active in the service for 4-6 months. However, they can be referred back at any point during the two years without additional cost to the provider (hospital/GP). Any unscheduled care need for an active patient is digitally monitored and automatically triggers the clinical coach to respond and provide remedial support. A clinical coach builds relationships, understands context and works alongside other healthcare professionals and services to focus on the most personalised care plan for each patient. One clinical coach has an active caseload of between 30-60 patients at any one time.
A randomised control trial pilot in NHS Vale of York Clinical Commissioning Group (CCG) with an ‘intervention group’ receiving HN Clinical Coaching saw a significant reduction in unplanned and planned hospital admissions and A&E attendances (23.7%, 24.1% and 34.1% respectively).
Patient feedback has been positive: “After my heart attack, I didn’t understand my symptoms. I was having panic attacks. The support from the health coach was excellent, she was outstanding, even after 18 months, I no longer have panic attacks and I am looking and feeling well. I was so anxious, and cardiologists didn’t have time, but working through this with a coach made a massive difference”.
I am delighted to be supporting another fantastic project within the programme. There are three implementation projects across the region, one of which is the first trial of the service in primary care with Selby Town and South Hambleton and Ryedale Primary Care Networks (PCN) in Vale of York.
- NHS North Yorkshire Clinical Commissioning Group (CCG) in collaboration with York Teaching Hospital NHS Foundation Trust started screening patients at the end of March and on-boarded patients early April and Harrogate and District NHS Foundation Trust started screening patients at the beginning of July.
- The Vale PCN networks in NHS Vale of York CCG started screening patients in April.
The project will benefit 1,000 patients in the Yorkshire and Humber region and help patients improve self-management of their conditions, avoiding unnecessary hospital admissions or visits to A&E.
We would like to acknowledge the support and collaboration from the project teams in Humber, Coast and Vale Health and Care Partnership and HN.
