Co-designing effective sickle cell services
Written by: Harriet Smith - 5th December 2023
Patient experience is fundamental to designing services that deliver effective care. When commissioning health and social care services and making changes to clinical pathways, it is crucial to listen to the voices of those with lived experience. These authentic voices offer decision-makers invaluable insights into how services affect patients, the challenges they encounter, and the obstacles they face in accessing the care they need.
In the UK, approximately 15,000 people have sickle cell disease, a debilitating condition causing painful crises, infections, and reducing life expectancy, profoundly impacting the lives of those affected. Automating red blood cell exchanges can help reduce the necessity for top-up transfusions, effectively manage pain, and lower the risk of experiencing multiple periods of intense pain a year – known as a crisis – due to blood clotting in their arteries.
As part of NHS England’s MedTech Funding Mandate policy, the Health Innovation Network was tasked with increasing access to Spectra Optia apheresis devices, one of the technologies supported through the programme, helping to address long standing inequalities reported by patients in accessing the right care.
In my role as National Programme Lead, I drive initiatives to increase the adoption of this medical technology. Through close collaboration with key stakeholders, including NHS England, the MedTech Funding Mandate team, NHS England Specialised Commissioning, NHS Blood and Transplant, Terumo, and the Sickle Cell Society, we aim to expand automated red blood cell services for sickle cell patients where they are most needed within the NHS and reduce health inequalities.
Recognising the significant challenges and barriers faced by patients with this condition in accessing necessary care, it was crucial to understand their experiences before implementing pathway changes. To achieve this, I partnered with NHS England’s Patient and Public Involvement and Engagement Team in the Innovation, Research and Life Sciences Group, Haemoglobinopathy Coordination Centres and the Sickle Cell Society to conduct a comprehensive national survey and a webinar. These efforts sought to unveil patients’ preferences, willingness to travel for treatment, and the obstacles hindering their access to essential care.
The need for change
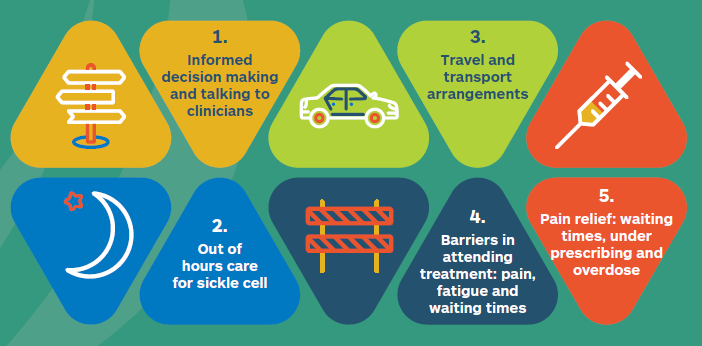
Analysis of the survey results and conversations during the webinar indicated a need for change across five priority areas within the sickle cell treatment pathway:
-
More emphasis on informed decision-making
26% of those affected by sickle cell felt that they had not made an informed decision to undertake automated red cell exchange during a conversation with a healthcare professional, nor had equal input into the discussions.
-
Better and more appropriate access to out of hours care
Receiving treatment out of hours is not unusual, as sickle cell is an unpredictable condition and patients could experience crisis at any time. The survey revealed that of those 121 patients attending out of hours, 34% needed a blood transfusion and a top up, but only 7% received an automated exchange. During the webinar, clinicians cited lack of available resources and capacity as major issues when treating patients out of hours, including access to medical devices, the availability of staff and even the physical space required to undertake the treatment which were all deemed to be barriers to providing optimal treatment.
-
More thought given to the impact of travel and transport
Anecdotal evidence highlighted the impractical extent of travel individuals were expected to undertake to receive their automated exchange treatment. The survey further validates those concerns, revealing that 55% of participants travelled for less than an hour, 31% for 1-2 hours, and 14% for over 2 hours.
The transport predominantly used was buses, cars and taxis. One of the respondents replying to this survey stated that they had “opted not to try automated exchange because of the amount of travel involved”
-
Greater understanding of the barriers in attending treatment: pain, fatigue and waiting times
Patients and carers told us about how a sickle cell patient presenting in crisis in the A&E should be seen quickly, perhaps directed to a more appropriate unit, which has capacity. Some responses suggested that capacity in these units needs to be increased.
-
The importance of effective pain relief: the wait, under prescribing and overdose
Although most sickle cell patients reported they tended to receive their pain medication ‘at once’ when attending the emergency department, when examining the responses, and after listening to patients’ experience, it was apparent that timely and adequate pain relief was something which really needs to be more fully addressed. There was a consensus during the webinar that the pain caused by this condition was not always understood by clinicians, leading patients to experience anxiety and vulnerability when seeking medical attention. This, in turn, acts as a significant barrier to their hospital attendance.
What next?
As part of this work, we have already implemented a number of initiatives. We have worked with Terumo and the Sickle Cell Society to produce an avatar in English and French to help patients understand their treatment options and how automated red blood cell exchange is not just for emergencies, but can be accessed routinely every few weeks by eligible patients.
We are currently helping all ten Haemoglobinopathy Co-ordination Centres across England to look at their sickle cell populations and devise cost effective options for the expansion of their services.
We are also working with NHS Blood and Transplant to deliver education and training to emergency department staff, enhancing their understanding of the disease and the specific needs of patients seeking care.
Read the full report to find out more about the findings of the patient survey and webinar.
