Community-led health checks
Written by: Adele Bunch - 31st October 2023
In this blog, Adele Bunch, our Head of Portfolio for health inequalities, mental health and patient and public involvement, highlights a successful project in West Yorkshire which is diagnosing cardiovascular disease and diabetes amongst its underserved populations by taking clinics to them.
All too often, our communities in Yorkshire and across the country, struggle to access primary care services and depending on local geography, language barriers, mobility, and transport availability and affordability, seeing a GP or even speaking to a healthcare professional can be much harder, if not impossible.
Health checks are crucial to our populations living well for longer. Without having routine height, weight, Body Mass Index, blood pressure and full bloods monitored, long-term treatable conditions such as cardiovascular disease (CVD) and diabetes can go undiagnosed which often result in preventable, sometimes fatal episodes, such as heart attack and stroke. It is estimated that around 7 million people in the UK have undetected high blood pressure, so the scale of the problem is significant.
For people who are unable to routinely access primary care, health conditions can manifest, health inequality widens and ultimately, people unnecessarily die younger. The emotional effect on people and their families, combined with the financial impact on the NHS, and the wider economic burden, must be considered if we are to move the dial.
So, how do healthcare systems improve primary care access for all, and meet the NHS England Core20PLUS5 aspirations in a pressurised environment with patient demand that often outstrips workforce capacity? Academics and clinicians in the city of Bradford in West Yorkshire are tackling this head on.
Bradford: the strength of community engagement
Bradford, with a population of around 547,000 as of 2021, houses some of the most deprived and diverse communities in England. But within this UK City of Culture lies strength and tenacity of its strong faith communities, led by engaging and proactive voluntary and community organisations who galvanise people, foster trust and who are supporting clinical colleagues in local primary care networks to carry out health checks on the community.
The Improvement Academy, part of the Bradford Institute for Health Research (BIHR) with the local community action group Bradford 4 Better, identified increased mortality and had conversations with community members that highlighted experience of poor outcomes from CVD. They talked with people, listened to their access needs, and decided to take health checks to them in familiar, friendly environments.
The model focuses on community health improvement through tailored health messaging, the community health check events, social prescribing, and accessible services. The event lasts approximately two hours and involves a team of nurses, healthcare assistants, and community volunteers. When abnormal results are detected, participants receive prompt follow-up from GPs. The programme also engages in social prescribing, connecting participants to resources addressing broader health determinants.
The impact of health check events
In February 2023, the first health check event was held at the Islamic Madni Centre, attracting over 100 people speaking six different languages, aged between 30-69, some came from out of area. 61% of attendees had abnormal blood pressure, with two immediately referred to emergency care.
News of the initiative travelled far and wide. A healthcare provider in Pakistan has since introduced the approach and the team have been shortlisted for the upcoming Health Service Journal Health Inequalities award.
Leveraging the success of the first session and supported by Health Innovation Yorkshire & Humber, phase 2 of the project is underway with subsequent health check events having taken place in August and September 2023.
The second session was held at the Girlington Community Centre and attracted 55 participants with 27% exhibiting abnormal blood pressure results. It also successfully engaged partner organisations including Diabetes UK, interacting with 32 attendees to provide valuable information on diabetes-related topics.
The third event took place at the Milat Islamia Mosque. This saw a substantial increase in attendance, with 86 individuals participating and 78 patient records documented. 41% of participants had abnormal blood pressure readings. The attendees included 56% with a known hypertension diagnosis and 43% with abnormal measurements but without prior diagnoses. Specifically, 45% of male participants had abnormal blood pressure readings, while 36% of female participants displayed abnormal results.
Anonymous community participant aged 50, from a BD5 postcode:
“During a local community health check event that my friends had organised, I received a diagnosis of hypertension. Although I had only gone to support them, the experience was quite unsettling as it made me realise the severity of my high blood pressure. However, I quickly sought medical attention from my GP and was prescribed medication to lower my blood pressure. This incident was a wake-up call that prompted me to make serious lifestyle changes, especially for the sake of my three young children. Although it is a gradual process, I am grateful to have received a warning to improve my health, as not everyone is so fortunate.
“These health events are crucial in our communities as many people may be unaware of the dangers of hypertension, also known as the ‘silent killer’ especially with the abundance of fast-food outlets serving unhealthy processed food”.
Additionally, anecdotal reports from participants provided valuable insights, including difficulties in accessing primary care services, experiences of seeking care abroad due to trust issues, and success stories of individuals taking proactive steps to address their health, including three participants urgently referred for same-day assessments due to significantly elevated blood pressure readings.
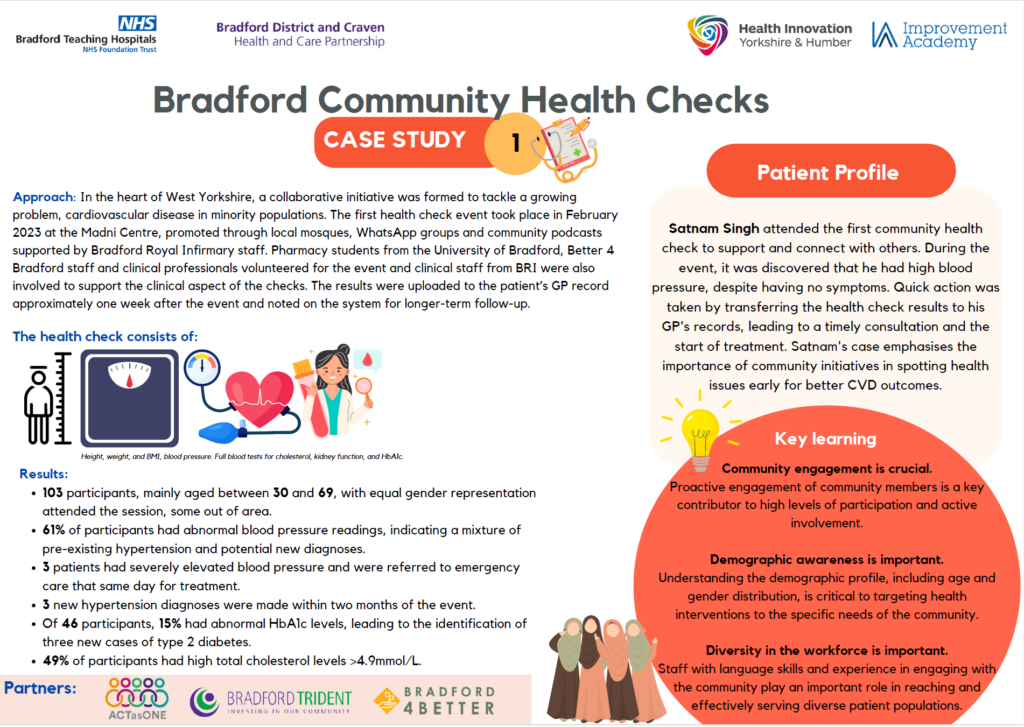
This infographic captures the project in a nutshell:
The future
As we continue to support this project that is going from strength to strength, we see great potential for the model to span into other clinical areas and patient cohorts. With long term investment, it has the capability to be a sustainable solution for primary care to improve patient access, experience and outcomes, save the NHS money and act as a one stop shop for assessing multiple patient needs. We will be supporting the development of a practical resource which harnesses the learning from this project to support other systems to adopt and scale.
For further information, please contact our project manager supporting this exciting work at vanessa.amoako@yhahsn.com.
