Medicines Safety
 About the programme
About the programme
The Medicines Safety Programme aims to significantly reduce severe avoidable harm and deaths linked to medication use. This initiative focuses on tackling the primary causes of severe harm associated with medicines, many of which have been longstanding issues yet persistently challenging our health and care systems. The programme affects safety culture, safety systems and high-risk medicines in common use. It brings the science of continuous safety improvement to bear on this complex problem.
In 2024/25 PSCs will continue to deliver the ‘Reduce harm from opioids in chronic non-cancer pain’ priority. Key principles for the delivery of this priority are:
- Considering the problem of high-risk opioids in chronic non-cancer pain from the perspective of the entire patient pathway is key and this requires system working.
- Managing chronic non-cancer pain requires personalised care and shared decision-making, focusing on providing patients with a combination of biopsychosocial support to help them live well with their pain. To make significant progress in this priority area, it is crucial to shift from the prevailing medical model of chronic pain management—which has led to high-risk opioid prescriptions for over one million people in England—towards a biopsychosocial model that includes supported self-management.
Who we are working with
We are working across Yorkshire and the Humber with ICS leads, Primary Care Networks, pharmacists, GPs, acute trusts, other clinicians, VCSE organisations, patients and the public to address the ambitions above.
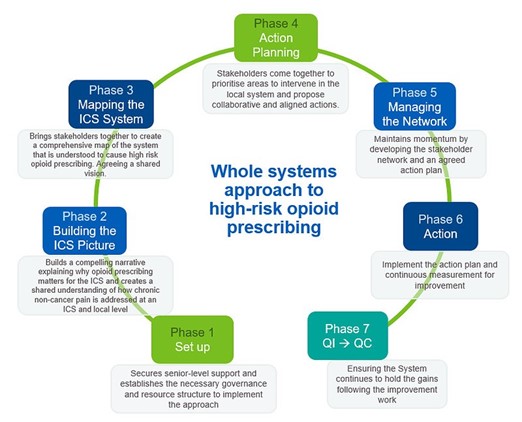
We are supporting ICS Medicines Optimisation teams in implementing a whole-systems approach to reducing harm from opioids in chronic non-cancer pain. The wider Health Innovation Network polypharmacy programme also supports this programme and we will continue to work in partnership throughout 2024/25.
Main deliverables
At least 50% of Integrated Care Boards across England are:
- Progressing through the phases of the whole-systems approach framework
- Identifying change ideas/initiatives with data to support adoption into business as usual and/or spread
- Providing visible and sustainable system leadership of this priority
Benefits
- 25,000 fewer people are prescribed oral or transdermal opioids (of any dose) for more than three months (NNH 62) compared to 31st March 2024, preventing approximately 400 deaths.
- 4,500 fewer people are prescribed high dose opioids (>120mg OME/day) compared to 31st March 2024 (aOR 2.2), halving their risk of opioid related death.
- People with chronic non-cancer pain reporting better quality of life, more able to be economically active and less disability because of improved care.
- Increase in availability, accessibility, awareness of and uptake of biopsychosocial offers including supported self-management.
Resource Library
We have set up a Yorkshire and Humber Medicines Safety Improvement Programme Padlet page to collate existing online resources on the subject of opioids and chronic pain management into one easy to access place.
This includes resources on topics such as:
- Patient and public education campaigns
- Patient information materials
- Patient stories
- Using data to identify patients at risk of harm
- Healthcare professional information and learning materials
- Social prescribing resources and services
- Measuring the impact of interventions
The library will be regularly reviewed and updated. Please share widely with your colleagues and do get in touch via the contact details below if you have any queries or any resources to add to the library.
How to get involved
Please contact:
Nicola Chicken, Project Manager
